Aptitude Health’s CORE events are designed to provide in-depth understanding of practice-specific patterns of care, disease-state treatment choices, and practice challenges and resource needs in different oncology and hematology indications. During the first 4 months of 2021, we conducted 8 different meetings among community oncologists and hematologists to gain insights into current practices in the management of follicular lymphoma (FL) and diffuse large B-cell lymphoma (DLBCL).
Lymphoma practice overview
In total, 70 community oncologists/hematologists participated. They were from a variety of practice sizes, as evidenced by the number of patients they have personally managed during the last 3 months; this ranged from 1–1000, with the majority (76%) seeing between 1–350 patients. Of these, 0–300 patients presented with hematologic malignances, and the majority (77%) of physicians reported seeing between 1–75 patients. While the number of patients with FL and DLBCL who had been treated fell between 0–50 and 0–60, respectively, most of the physicians had managed between 2–20 patients with FL and between 1–20 patients with DLBCL (84% and 87%, respectively). Collectively, participants had seen just over 16,000 patients over the last 3 months, of which ~24% had hematologic malignancies; there was a similar incidence of FL (~16%) and DLBCL (~15%).
Management of follicular lymphoma
Over two-thirds of physicians use formal criteria (Groupe d’Etude des Lymphomes Folliculaires [GELF], Follicular Lymphoma International Prognostic Index [FLIPI]-2, or FLIPI-1) to guide their decisions regarding whether to initiate treatment for patients with FL
Physicians favor regimens containing rituximab for the first- and second-line treatment of patients with FL; the anti-CD20–targeting agent obinutuzumab (in the first-line setting) and the immunomodulator lenalidomide (in the first- and second-line settings) are also popular choices
There is no single endpoint that physicians associate with improved overall survival (OS) in patients with FL
Participants were asked which drugs they had used to treat patients with FL during the last 3 months, to gain insight into the current management strategies for this disease. Obinutuzumab was the most commonly used drug, with 63% of participants having chosen it to treat a total of 102 patients, followed by lenalidomide, which was used by 60% of physicians to treat a total of 117 patients. Idelalisib had been selected by 19% of respondents, with ofatumumab and 90Y-ibritumomab tiuxetan rarely used (6% and 1.4%, respectively), and lutetium-177 lilotomab satetraxetan not used at all during the past 3 months.
The majority of physicians (66%) stated that maximizing progression-free survival (PFS) is their primary treatment goal for a newly diagnosed patient with FL. The second most common aim is minimizing toxicity while still offering active treatment (18.5%); very few respondents have the goal of achieving a clinical complete response (8.5%) or a fluorodeoxyglucose (FDG)-positron emission tomography (PET)–negative response (7.0%). There was no clear consensus about which endpoint is associated with improved OS in patients with FL. When asked to consider the options of PFS, minimal residual disease negativity, and FDG-PET negativity, there was no single endpoint that the majority of physicians consider to be solely associated with OS, although 60% of respondents cited that all 3 parameters could correlate with survival benefits.
To gain an understanding of how community oncologists/hematologists manage FL, participants were presented with the following patient case and then asked about their treatment decisions in various scenarios.
FL patient case
- 63-year-old man
- Lymphadenopathy noted 6 weeks earlier; node was 2 cm and unresponsive to antibiotics
- ENT surgeon performed excisional lymph node biopsy and diagnosed with grade 1–2 FL
- Patient referred to you; no B symptoms but had fatigue
PET scan reveals widespread adenopathy with disease in L axilla, mediastinum, porta hepatis, retroperitoneum, mesentery, and iliac chains bilaterally - Largest nodal mass is in the mesentery at 8 cm
- Iliac nodes are 6 cm in longest axis
- Other nodes range from 2 to 4 cm
- SUVmax is 10.8; LDH, normal; blood counts, normal; marrow not involved; no significant comorbidities
ENT, ear, nose, throat; LDH, lactate dehydrogenase; SUVmax, maximum standard unit value.
Physicians were asked which criteria they would use when deciding whether to initiate treatment for patients with FL. In total, 64% of respondents use some form of formal criteria to determine treatment initiation (GELF [27%], FLIPI-2 [23%], or FLIPI-1 [14%]), while a third (33%) stated they would only treat if the patient is symptomatic. The preferred treatment option for this FL patient case was bendamustine-rituximab (chosen by 87% of physicians); other treatment options included rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone (R-CHOP; 7%), lenalidomide-rituximab (R2; 3%), and cyclophosphamide, doxorubicin, obinutuzumab, prednisolone, vincristine (O-CHOP) or bendamustine-obinutuzumab (1.4% each). Overall, 73% of physicians would offer the patient maintenance therapy with rituximab if the patient achieved a good response to their initial treatment option.
Participants were then asked how they would treat the patient in the following scenario
- Complete response was achieved after frontline bendamustine-rituximab followed by maintenance rituximab, but the patient relapsed at the age of 66
- Biopsy revealed grade 1–2 FL, and the patient was observed for 1 year, but eventually the disease progressed enough to warrant a second line of therapy
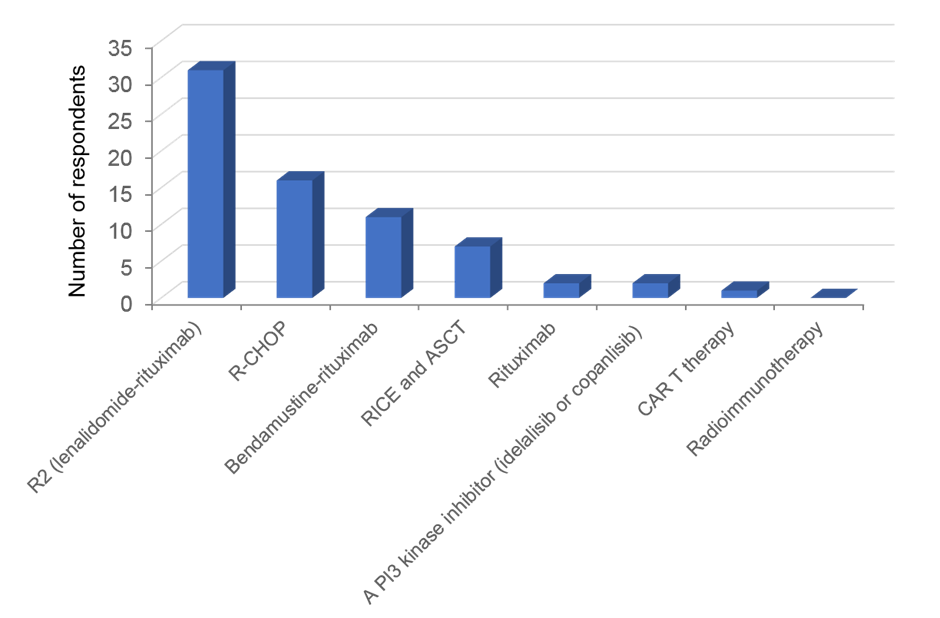
Figure 1 summarizes the responses to this question. While there was no consensus about one particular therapy, it was perhaps unsurprising that the most popular options all featured rituximab; newer therapeutic options, such as PI3 kinase inhibitors and CAR-T therapy, have yet to gain popularity.
Figure 1. Preferred second-line treatment options for a patient with FL.
ASCT, autologous stem cell transplant; RICE, rituximab, ifosfamide, carboplatin, etoposide.
Management patterns for diffuse large B-cell lymphoma
The presence of double- or triple-hit disease, and not the cell of origin, is considered an important factor when selecting treatment for patients with DLBCL by most physicians
Rituximab-containing regimens are the preferred management strategies in the first- and second-line settings for DLBCL
Participants were asked about the importance of the cell of origin when selecting treatment for patients with DLBCL. The responses were varied: 44% stated that they do check the origin of the malignancy, but it does not impact their treatment selection; 39% take the cell of origin into account when deciding on the most appropriate treatment; and 17% do not consider cell of origin an important factor. The impact of cell origin, age, performance status, and presence of double- or triple-hit disease features on treatment choice were also evaluated. The responses are summarized in Figure 2; the most impactful was double- or triple-hit disease features.
Figure 2. The impact of various factors on treatment choice in patients with DLBCL.
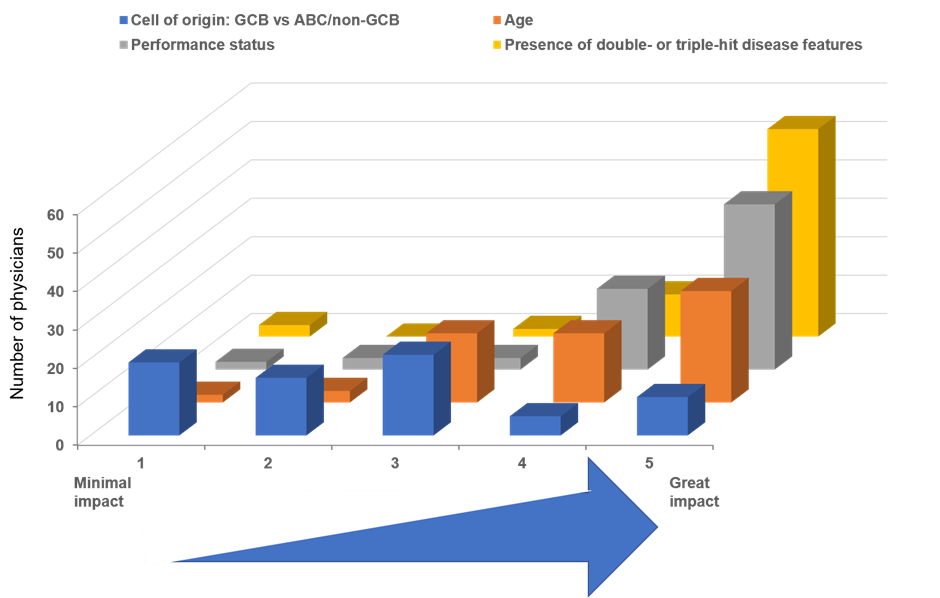
ABC, activated B-cell–like; GCB, germinal center B-cell–like.
To gauge community practice patterns in the management of DLBCL, a hypothetical patient case was presented.
DLBCL patient case
- 63-year-old man presents with 4-week history of back pain
- Imaging revealed 11-cm retroperitoneal mass; biopsy determined DLBCL, non-GCB (by Hans methods)
- IHC for bcl-2 and myc show high expression but FISH testing for bcl-2 and myc are negative; bcl-6 is positive
- PET imaging reveals widespread pathologic adenopathy with involvement of mediastinal, retroperitoneal, and mesenteric nodes
- 2 PET-avid mass lesions in liver; 1 lesion in left kidney
- No apparent marrow involvement
- SUVmax is 28; Ki67 is 90%; LDH 3× ULN
- PS = 1; no significant comorbidities
FISH, fluorescence in situ hybridization; IHC, immunohistochemistry; PS, performance status; ULN, upper limit of normal.
Participants were asked what the patient diagnosis would be, according to World Health Organization guidance; the majority (70%) stated the patient had DLBCL, whereas 30% diagnosed the patient with high-grade B-cell lymphoma with rearrangements of myc and bcl-2 and/or bcl-6. When asked about the risk of relapse in the central nervous system (CNS) for this patient, the responses varied. While the majority of physicians suggested the CNS IPI score was 3 (21%) or 4 (47%), 13% suggested the score was 5, 9% thought it was 2, 7% stated 6, and 1% thought the score would be CNS IPI 1. There was also no clear consensus between the physicians as to which treatment they would recommend for this patient (Figure 3).
Figure 3. Preferred first-line treatment options for patients with DLBCL.
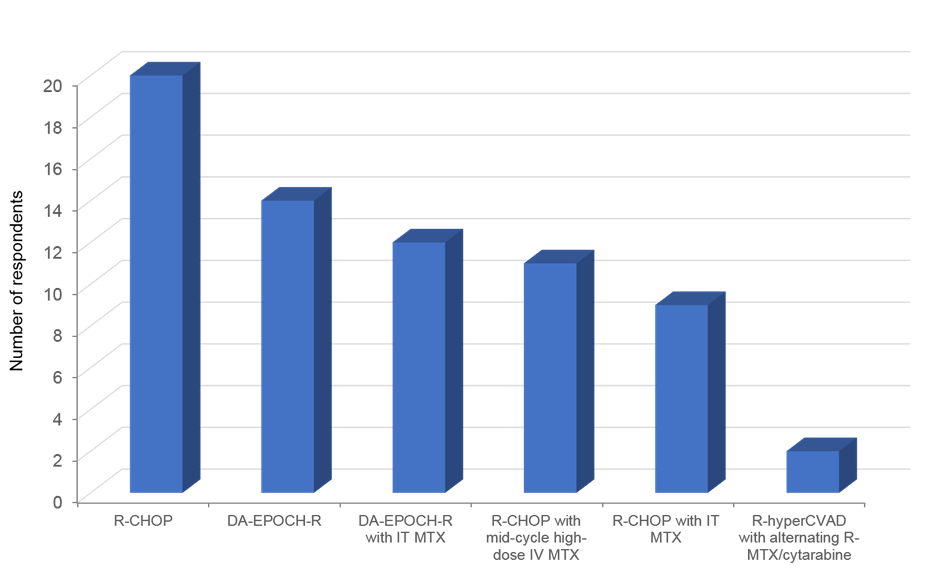
DA-EPOCH-R; dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab; IT, intrathecal; IV, intravenous; MTX, methotrexate; R-hyperCVAD, rituximab plus hyperfractionated cyclophosphamide, vincristine, adriamycin, dexamethasone; R-MTX, rituximab, methotrexate.
Respondents were also asked whether they would recommend ASCT consolidation if the patient achieved a complete response to frontline therapy; only 33% replied that they would take this approach. Physicians were then presented with a scenario in which the patient described above relapsed 1 year following completion of frontline R-CHOP treatment with confirmed DLBCL, and asked what their preferred treatment option would be. In this instance, the majority (79%) of respondents would recommend RICE followed by ASCT. Other options included entering the patient into a clinical trial (7%), R-DHAP followed by ASCT (6%), RICE followed by allogeneic (allo)SCT (93%), and CAR T therapy (1%); no respondents recommended the use of R-DHAP followed by alloSCT for this patient.
Finally, the majority of community hematologists (94%) do not use maintenance therapy in DLBCL and have never used radioimmunotherapy, such as ibritumomab tiuxetan, outside of a protocol setting.
In summary, when deciding on treatment options for patients with FL, most physicians rely on formal criteria, such as GELF, to help guide their choice. For patients with DLBCL, the presence of double- or triple-hit disease features are the most impactful when determining the optimal treatment strategy. Regimens containing rituximab remain the treatment of choice in the first- and second-line settings for patients who present with FL or DLBCL. For patients with FL, anti-CD20 antibodies and the immunomodulatory agent lenalidomide are also gaining popularity in the first-line setting.