In the latest of our series of expert oncologist interviews, Dr Omid Hamid, chief of research and immuno-oncology, co-director of the cutaneous malignancy program, and director of the melanoma and phase I programs at The Angeles Clinic and Research Institute, a Cedars-Sinai Affiliate in Los Angeles, CA, discussed recent advances in the field of melanoma.
In the latest of our series of expert oncologist interviews, Dr Omid Hamid, chief of research and immuno-oncology, co-director of the cutaneous malignancy program, and director of the melanoma and phase I programs at The Angeles Clinic and Research Institute, a Cedars-Sinai Affiliate in Los Angeles, CA, discussed recent advances in the field of melanoma.
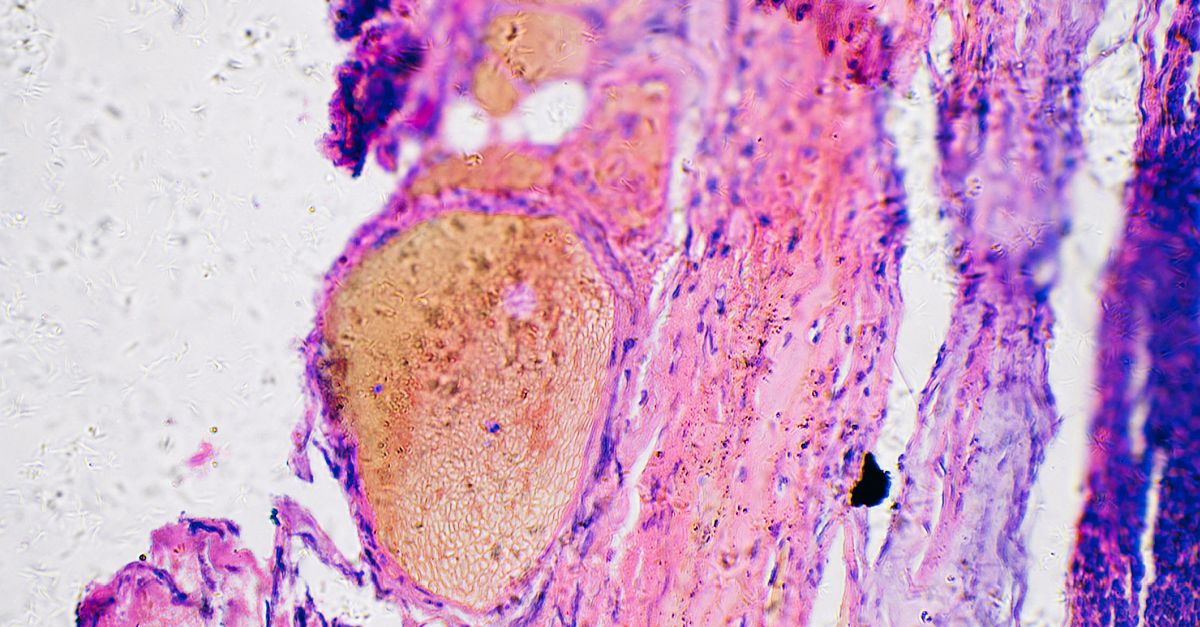
Melanoma continues to be a therapeutic challenge. The immunogenic nature of melanoma has made it an ideal proving ground for the development of immunotherapies, initially with cytokines and then with more-targeted approaches. In recent years, the immune checkpoint inhibitors (ICIs) anti-programmed cell death 1 protein/ligand 1 (PD-[L]1) and anti-cytotoxic T-lymphocyte antigen-4 (CTLA-4) monoclonal antibodies have become therapies of choice for metastatic melanoma. However, while these agents can mobilize the immune system, they are unable to direct the immune response against the antigens that are specific to the tumors (cancer neoantigens), and many patients are left with few options when ICIs fail.
Dr Hamid discussed an investigational immunotherapy that could potentially bridge this gap in the therapeutic continuum for melanoma, RP1 (vusolimogene oderparepvec). This oncolytic virus-based therapy selectively replicates in tumor cells and generates an immune cell-activating factor (granulocyte-macrophage colony-stimulating factor), leading to increased immunogenic death of melanoma cells. Insights on the potential of intratumoral injection of RP1 in combination with nivolumab in patients with melanoma for whom prior ICI therapy has failed were revealed at the 2023 American Society of Clinical Oncology Annual Meeting in a snapshot readout of the multi-arm phase I/II IGNYTE study (NCT03767348) in adult patients with advanced and/or refractory solid tumors. In the 91-patient cohort of those with cutaneous melanoma who had prior ICI therapy and received the RP1 + nivolumab combination, the overall response rate (ORR) was 37.4%. Adverse events were predominantly “on-target” flu-like grade 1–2 side effects indicative of systemic immune activation. Responses were seen not only in the injected tumors but also at other sites, possibly through immunogenic neoantigen release during viral lysis of the cancer cells providing specific targets. This could generate systemic cancer neoantigen recognition and antitumor immune response.
In December 2023, updated IGNYTE data were released from 156 patients who had disease progression either during or after completion of anti–PD-1 therapy and were treated with RP1 + nivolumab. In these patients, the ORR was 31.4% with a complete response (CR) rate of 12%, showing activity consistent with the prior snapshot of 91 patients in this cohort. Responses were seen across disease stages, including CRs in patients with stage IVM1b/c disease. Responses are highly durable, with median duration of response greater than 24 months, and often deepening over time. Adverse Events were consistent with the known profiles of immunotherapy regimens.
Watch the full interview here: