Brain metastases in patients with breast cancer vary in prevalence and timing. Prognosis is generally poor for patients with brain metastases, so proper and timely management is critical. Knowledge of risk factors that impact the timing of brain metastasis may help guide appropriate follow-up care for patients with breast cancer.
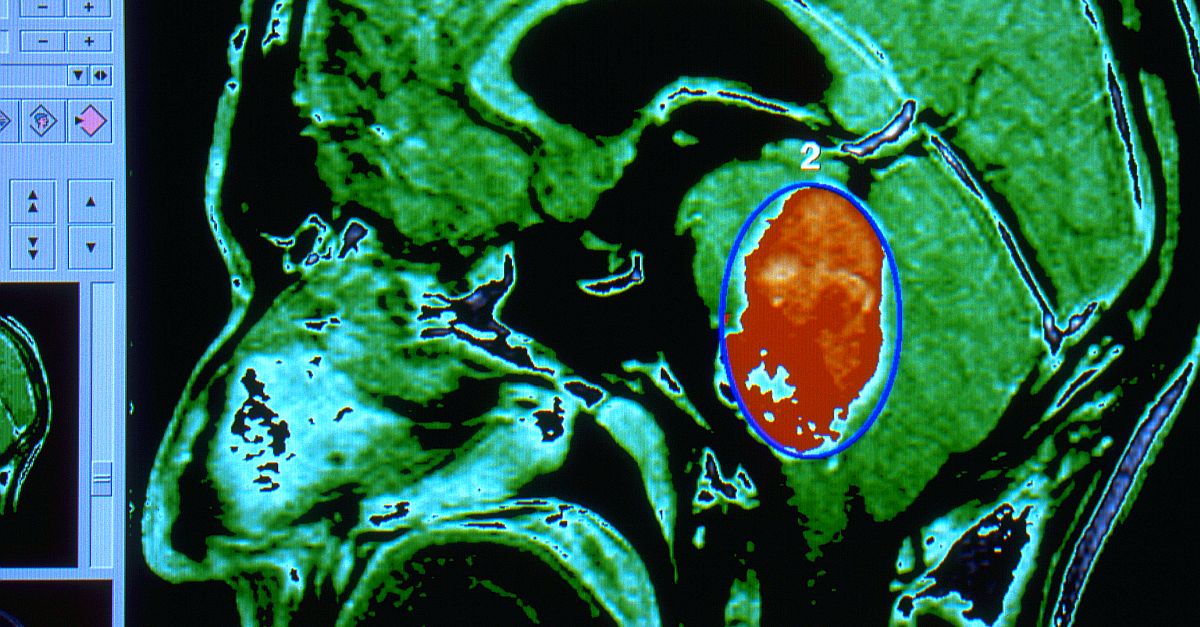
A team of experts at the University Hospital Essen in Germany analyzed 93 patients who underwent breast cancer surgery, to identify predictors associated with the time interval of brain metastasis occurrence and determine the impact of time interval on overall survival after surgery in these patients. The patients’ median age was 52 years, and the median time interval from initial breast cancer diagnosis to brain metastasis was 45 months. Median overall survival following brain metastasis surgery was 16 months. Time to brain metastasis of less than 5 years was significantly associated with decreased overall survival, midline shift in preoperative magnetic resonance imaging, and identic estrogen receptor status. Other independent predictors of postoperative survival following brain metastasis surgery were age 65 years or older at breast cancer diagnosis, initial higher breast cancer grade stage, breast cancer treatment with trastuzumab, tumor necrosis in preoperative magnetic resonance imaging, and adjuvant brain radiation.
Among breast cancer-related characteristics, Union for International Cancer Control (UICC) stage III or IV was an independent predictor of a shorter time interval (<5 years) to brain metastasis. The analysis also showed the impact of breast cancer subtype on the timing of brain metastasis. Invasive ductal breast cancer was prone to an earlier occurrence of distant metastases, possibly due to an increased collective epithelial invasion. Conversely, invasive lobular breast cancer is characterized by a higher rate of cell individualization, which resulted in a longer time to development of distant metastasis for patients with this tumor type. Late occurrence (≥10 years) of brain metastasis was found in 15 (16.1%) patients and was associated with invasive lobular breast cancer subtype and adjuvant breast radiation. Among those with late brain metastases, there was a higher proportion of patients who had mastectomy with no radiation afterward. The authors suggested this may be because in patients undergoing breast-conserving surgery, there is a possibility of residual tumor cells sprouting into the vascular and lymph nodal system and influencing the risk and timing of distant metastases. Because irradiation of tumor cells increases the growth capacity and the transformation process, adjuvant radiation could promote molecular changes in residual tumor cells that potentially lead to development of aggressive and resistant breast cancer.
High level
These findings suggest that protocols for patient follow-up should take an individualized approach, rather than following a 10-year limit. Further studies are needed to increase understanding of the complex cellular pathways behind the timing of brain metastasis and survival prognosis in individuals with breast cancer. Researchers can help to advance this knowledge by conducting studies in larger populations and in different breast cancer subpopulations to confirm these results and help guide patient follow-up.
Ground level
Higher age, tumor subtype, trastuzumab therapy, brain radiation, and tumor necrosis are survival predictors for patients with breast cancer and brain metastases undergoing surgery. In particular, initial breast cancer stage (UICC) may be a critical factor influencing the survival effect of time interval on the prognosis of brain metastasis surgery. These predictors highlight the importance of an adjusted, patient-specific follow-up strategy based on initial tumor characteristics and previous treatment, not limited to 10 years. In particular, patients with invasive lobular breast cancer and without initial adjuvant breast radiation were more likely to have later onset of first distant brain metastases and should be considered for longer follow-up.