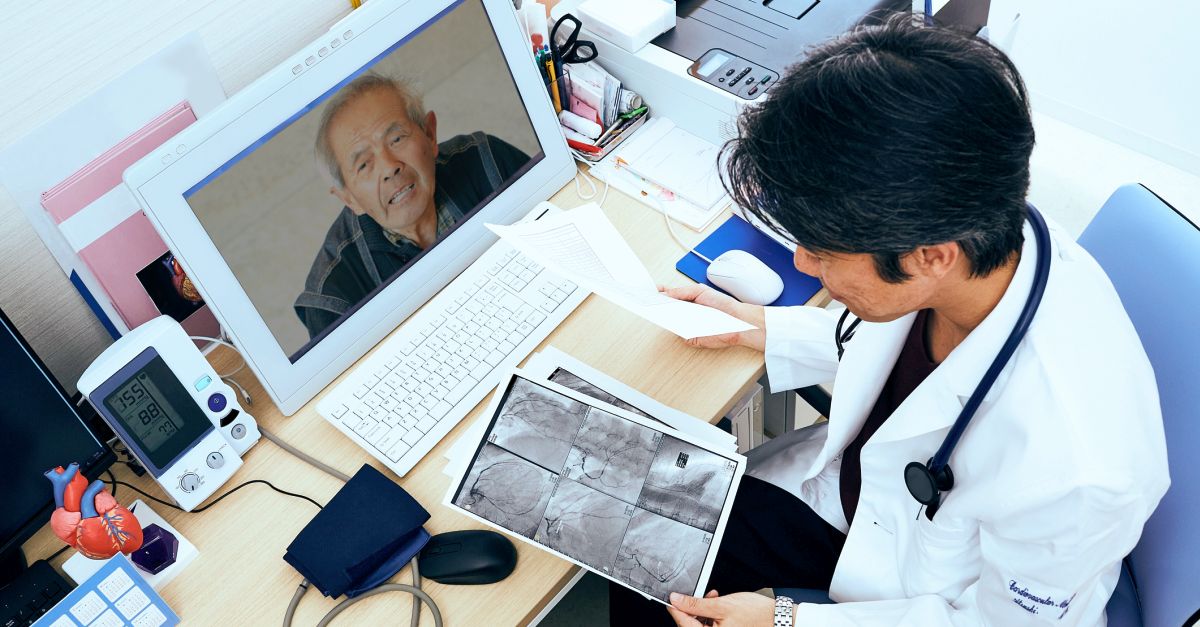
Interest in and access to telemedicine has gained momentum in recent years, especially during the COVID-19 pandemic. New diagnostic and communication technologies have greatly improved the capabilities and quality of available interventions. In fact, studies have demonstrated that telemedicine is equivalent to—or at times, achieves better outcomes than—in-person care, with improved cost-effectiveness, greater convenience, and high levels of patient and healthcare professional satisfaction. With regard to oncology, the predicted shortage of oncologists in the United States, aging of the population, and logistic challenges provide strong rationale for the use of telehealth services. In an American Society of Clinical Oncology Educational Book, Dr S. Joseph Sirintrapun and Dr Ana Maria Lopez summarized available technologies and their tremendous potential in facilitating care for patients with cancer. Among these interventions are telegenetics, telepathology, bundling of cancer-related teleapplications, survivorship care, and novel approaches to increasing access to clinical trials.
Virtual solutions are particularly impactful for sites requiring extended travel time. For some patients, a blend of in-person and virtual options can provide a pathway to optimal care, as this approach helps bring multidisciplinary team-based care to a wider segment of patients. Recent teleoncology service innovations include remote supervision of chemotherapy delivery and use of portable, home-based, and mobile technologies for home health follow-up such as wound care, symptom management, and palliative care. Additionally, telepathology is being applied to rapid on-site evaluation (ROSE) with real-time telecytology (TC). The authors describe 2 large-scale models for synchronous real-time TC operations for ROSE developed by Memorial Sloan Kettering Cancer Center: 1 uses robotic microscopes controlled by off-site cytotechnologists, and 1 uses streaming of high-definition video microscopy. Tele-education and virtual tumor boards also have a growing role in oncology, helping to build and support the oncology workforce both in urban and rural settings and across disciplines.
High level
Digitalization of health records and virtual diagnostic tools improves the exchange of health information and contributes to the success of teleoncology practices. When adopting these practices, there must be procedures in place to maintain professional standards, such as making sure full documentation is integrated into the patient’s electronic health record. Training is essential to help clinicians continue to facilitate rapport, maximize engagement, and conduct an accurate exam. De-identified health information can also be exchanged electronically for unprecedented access to population-based data. However, there will be discrepancies between institutions regarding their ability to apply teleoncology practices. Given that technologies are changing rapidly, the authors recommend using the best technology that the institution can afford to stay close to the leading edge.
Ground level
In the US, reimbursement for telemedicine varies, so clinicians must be sure to understand the current rules in their own state. For example, Medicare considers a patient’s location when determining reimbursement. Always check a patient’s insurance coverage, as individual insurance plans may vary as well. Interested clinicians can contact the National Consortium of Telehealth Resource Centers at www.telehealthresourcecenter.org for the latest information on telemedicine reimbursement, parity, and practice.