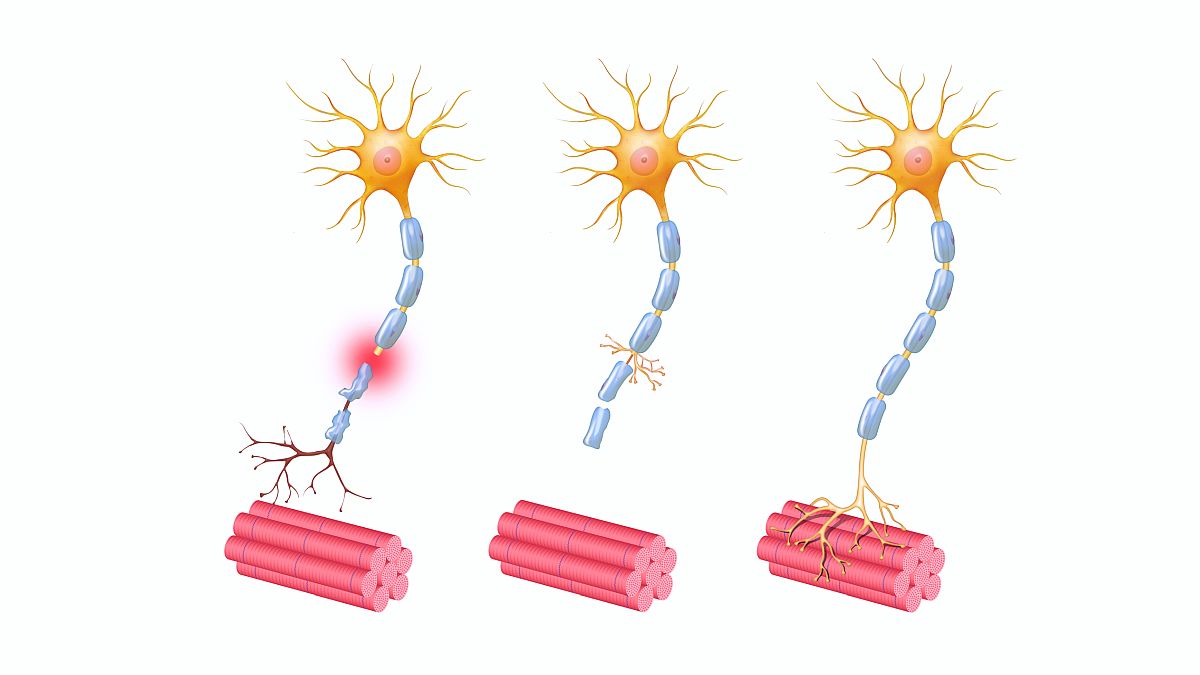
Chemotherapy-induced peripheral neuropathy, or CIPN, is a common adverse reaction associated with anticancer agents used for multiple tumor types, such as taxanes, platinums, vinca alkaloids, proteasome inhibitors, and immunomodulatory agents. Clinical onset varies, with presentation as sensory, motor, or autonomic effects, and symptoms do not always improve with cessation of therapy, sometimes leading to a decreased quality of life. Therefore, patients receiving chemotherapy may benefit from approaches to prevent or treat CIPN.
To help address this ongoing concern, the American Society of Clinical Oncology (ASCO) released updated clinical guidelines for prevention and management of CINP in July 2020. These guidelines were recently summarized in a synopsis for the Journal of the American Medical Association by Dr Benjamin A. Derman and Dr Andrew M. Davis. Overall, the recommendations were focused more on what is not recommended than on what is, with strong recommendations against several agents, including acetyl-L-carnitine, pregabalin, and venlafaxine. The guidelines do provide a moderate recommendation for patients with disabling or intolerable CIPN, suggesting dose delay, reduction, or chemotherapy cessation, but this is based on expert opinion without supporting data. For patients with painful CIPN, the guidelines recommend duloxetine on the basis of the results from 3 clinical trials. Other exploratory treatment options that may have benefit but are not sufficiently supported by clinical trial data include physical activity, acupuncture, scrambler therapy, pregabalin/gabapentin, topical gel treatments, tryicyclic antidepressants, and oral cannabinoids.
The European Society for Medical Oncology (ESMO) also released guidelines in 2020, and those guidelines suggest consideration of venlafaxine or antidepressants for treatment of CIPN if duloxetine has failed. Because of their low risk of harm, the ESMO guidelines also include weak recommendations for topical local interventions and nonpharmacologic interventions such as acupuncture, active lifestyle, and neurofeedback.
High level
There is an overall lack of evidence supporting various approaches for CIPN prevention and management. Clinical research is clearly needed, and researchers should explore the potential benefit of alternate treatment options (eg, duloxetine, sphingosine-1-phsopate receptor-1 targeted agents, and physical activity) in patients who are at risk for or have symptoms of CINP. The authors also suggested that genetic analysis paired with CIPN phenotype and other clinical factors from patients in clinical trials could potentially be used to help predict susceptibility to developing CIPN and establish tailored strategies for at-risk patients.
Ground level
As with all treatments, when making decisions about prevention or management of CINP, clinicians need to carefully consider the potential benefits versus the risks. The ASCO guidelines discourage the use of therapies that have little to no proven benefit and with potential harm. While the guidelines suggest use of duloxetine to treat CIPN, clinicians must weigh the benefits against the potential adverse events, which include weight loss, anorexia, nausea, fatigue, and headaches. Caution should also be taken when delaying, reducing, or stopping chemotherapy, as these approaches may compromise treatment of the underlying cancer. The authors suggest empowering primary care clinicians to discuss interventions with the treating oncologist and/or a clinician trained in pain medicine, as they are well suited for a role as first-line patient advocates and may be able to help support quality-of-life measures.